Guang Yang
Exercise and Sport Sciences Program, Graduate School, Khon Kaen University, Khon Kaen 40002, Thailand
Narisara Premsri
Exercise and Sport Sciences Development and Research Group, Khon Kaen University, Khon Kaen 40002, Thailand
Terdthai Tong-un
Faculty of Medicine, Khon Kaen University, Khon Kaen 40002, Thailand
Rujira Nonsa-ard
Faculty of Public Health, Mahasarakham University, Mahasarakham 44150, Thailand
Ploypailin Aneknan
Exercise and Sport Sciences Development and Research Group, Khon Kaen University, Khon Kaen 40002, Thailand
Orathai Tunkamnerdthai
Faculty of Medicine, Khon Kaen University, Khon Kaen 40002, Thailand
Apiwan Manimanakorn
Faculty of Medicine, Khon Kaen University, Khon Kaen 40002, Thailand
Naruemon Leelayuwat
Exercise and Sport Sciences Program, Graduate School, Khon Kaen University, Khon Kaen 40002, Thailand
DOI: https://doi.org/10.14456/apst.2025.59
Keywords: Aerobic exercise Ageing Cardiorespiratory fitness Respiratory muscle strength Ventilatory efficiency
Abstract
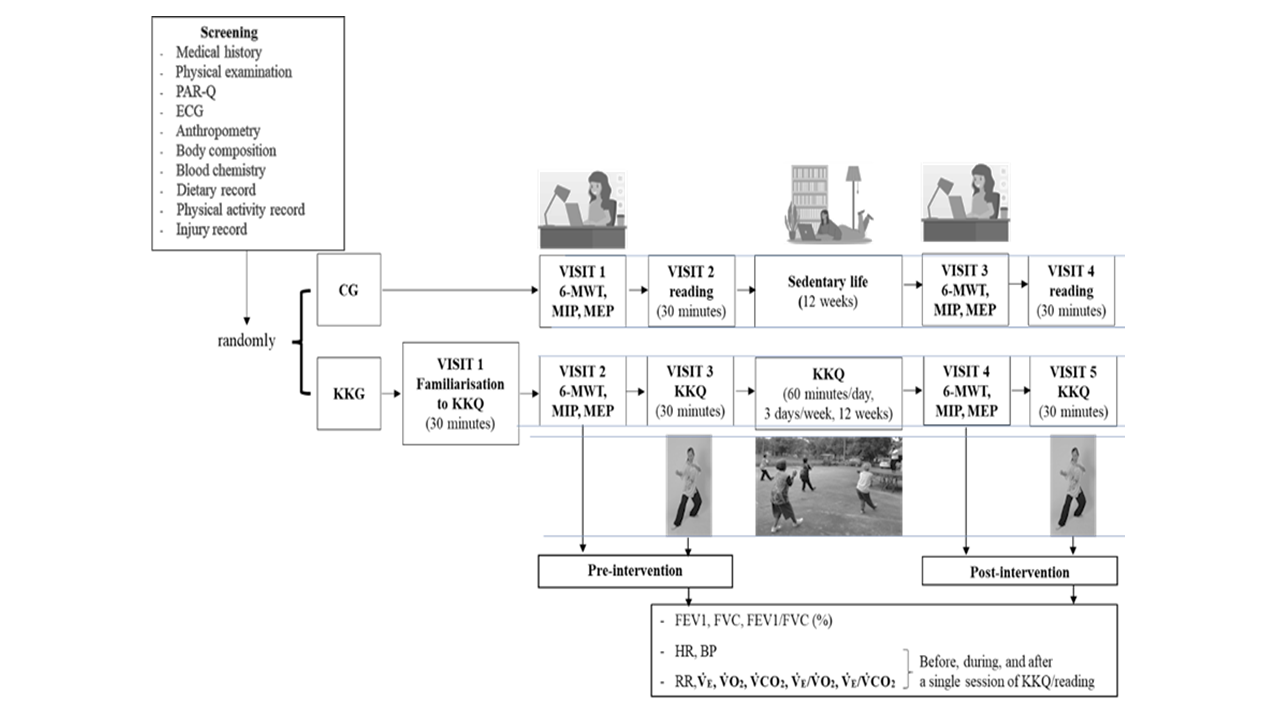
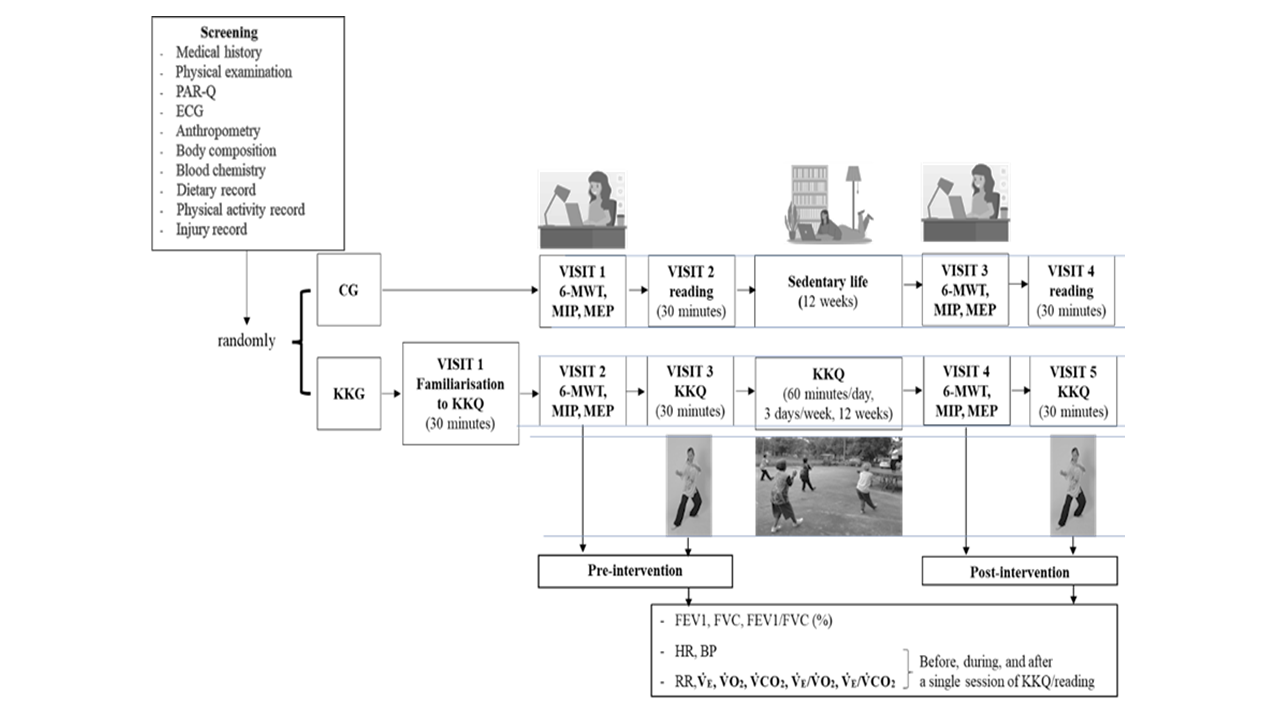
This study investigated the acute and training effects of Khon Kaen Qigong (KKQ), which combines Qigong and Muay Thai, on the cardiopulmonary responses in older adults. There were two experiments: 1) acute effect: a 30-minute KKQ session (control group performed reading) at pre-intervention and, 2) training effect (post-intervention compared with pre-intervention): composed of two conditions: the single session of KKQ/reading and two tests of cardiorespiratory fitness and respiratory muscle strength. Training intervention consisted of a 60-minute KKQ/day, three days a week (the control group had a sedentary life) for 12 weeks. At pre-intervention, there were three days of the experiment: 1) familiarization with the KKQ session, 2) heart rate, blood pressure, pulmonary function, and expired gas collection in response to KKQ/reading, and, 3) the six-minute walk distance and respiratory muscle strength. Post-intervention, participants repeated the pre-intervention except familiarization day. We found that the training contributed to a greater six-minute walk distance compared to the control group (mean difference [95%CI]; 7.04 [-14.94, 29.02], p < 0.05). Compared to the reading, it increased oxygen consumption (p < 0.05) and decreased ventilatory efficiency (p < 0.05) during and after the 30-minute KKQ session. The acute KKQ session produced cardiopulmonary responses to a very low level. An improvement of walking distance and ventilatory efficiency were previously shown to be negatively associated with cardiovascular risk and mortality. Thus, KKQ could be an alternative exercise that should be promoted to enhance a healthy long life for the older participants.
How to Cite
Yang, G., Premsri, N., Tong-un, T., Nonsa-ard, R. ., Aneknan, P. ., Tunkamnerdthai, O. ., Manimanakorn, A. ., & Leelayuwat, N. (2025). Effects of Qigong combined with Wai Khru Muay Thai on cardiopulmonary responses in sedentary older adults: A randomized control trial. Asia-Pacific Journal of Science and Technology, 30(04), APST–30. https://doi.org/10.14456/apst.2025.59
References
Yang G, Premsri N, Tong-un-T, Tunkamnerdthai O, Manimmanakorn A, Nonsa-ard R, et al. Effects of Qigong combined with Muay Thai on cardiorespiratory responses and exercise intensity in sedentary older participants. Arch AHS. 2024;36(1):12-22.
Liu G, Premsri N, Tong-un-T, Sespheng A, Teparak C, Nonsa-ard R, et al. Acute effect of novel mind-body exercise on heart rate variability in older adults. JEP online. 2022; 25:51-69.
Liu G, Premsri N, Tong-un-T, Aneknan P, Tunkamnerdthai O, Muktabhant B, et al. Training effects of novel mind-body exercise on physical fitness and psychological responses in older adults. JEP online. 2023;26(1):12-30.
Population Division, DESA, United Nations PUBLICATIONS. World Population Aging 1950–2050. [Internet]. 2002 [cited 2025 Jan 24].
Lin H, Wan M, Ye Y, Zheng G. Effects of Baduanjin exercise on the physical function of middle-aged and elderly people: a systematic review and meta-analysis of randomized controlled trials. BMC Complement Med Ther. 2023; 23:38.
Saraiva BTC, Franchini E, Ribeiro AS, Gobbo LA, Correia MA, Vanderlei LCM, et al. Effects of 12 weeks of functional training vs. Muay Thai on cardiac autonomic modulation and hemodynamic parameters in older adults: a randomized clinical trial. BMC Cardiovasc Disord. 2024;24(1):433.
Yang WY, Xu Y, Ye L, Rong LJ, Feng J, Huang BL, et al. Effects of Baduanjin exercise on quality-of-life and exercise capacity in patients with heart failure: A systematic review and meta-analysis. Complement Ther Clin Pract. 2023; 50:101675.
Li L, Huang H, Song J, Yu Y, Jia Y, Wang Y, et al. Network meta-analysis of the effects of different types of traditional chinese exercises on pulmonary function, endurance capacity and quality of life in patients with COPD. Front Med (Lausanne). 2022; 9:806025.
Wang K, Liu S, Kong Z, Zhang Y, Liu J. Mind-Body Exercise (Wuqinxi) for Patients with Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int J Environ Res Public Health. 2018; 16:72.
Dourado VZ, Nishiaka RK, Simões MSMP, Lauria VT, Tanni SE, Godoy I, et al. Classification of cardiorespiratory fitness using the six-minute walk test in adults: Comparison with cardiopulmonary exercise testing. Pulmonology. 2021;27(6):500-508.
Kabisch M, Ruckes C, Seibert-Grafe M, Blettner M. Randomized controlled trials: part 17 of a series on evaluation of scientific publications. Dtsch Arztebl Int. 2011;108(39):663-668.
Chan AWK, Lee A, Suen LKP, Tam WW. Tai chi Qigong improves lung functions and activity tolerance in COPD clients: A single blind, randomized controlled trial. Complement Ther Med. 2011; 19:3–11.
Lan C, Chou SW, Chen SY, Lai JS, Wong MK. The aerobic capacity and ventilatory efficiency during exercise in Qigong and Tai Chi Chuan practitioners. Am J Chin Med. 2004;32(1):141-150.
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002; 166:111–117.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005; 26:319-338.
American Thoracic Society/European Respiratory Society. ATS/ERS statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002; 166:518-624.
Enright PL, Kronmal RA, Manolio TA, Schenker MB, Hyatt RE. Respiratory muscle strength in the elderly. Correlations and reference values. Cardiovascular health study research group. Am J Respir Crit Care Med. 1994;149(2 Pt 1):430-438.
Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, et al. American College of Sports Medicine. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334-1359.
Feng F, Tuchman S, Denninger JW, Fricchione GL, Yeung A. Qigong for the Prevention, Treatment, and Rehabilitation of COVID-19 Infection in Older Adults. Am J Geriatr Psychiatry. 2020 28:812-819.
Perrey S. Muscle Oxygenation Unlocks the Secrets of Physiological Responses to Exercise: Time to exploit it in the training monitoring. Front Sports Act Living. 2022; 4:864825.
Tsai WJ, Tsai HY, Kuo LY, Lin YS, Chen BY, Lin WH, et al. VE/VCO2 Slope and functional capacity in patients post-heart transplantation. Transplant Proc. 2018;50(9):2733-2737.
Ross R, Blair SN, Arena R, Church TS, Després J-P, Franklin BA, et al. American Heart Association Physical Activity Committee of the Council on L, Cardiometabolic H, Council on Clinical C, Council on E, Prevention, Council on C, Stroke N, Council on Functional G, Translational B and Stroke C. Importance of assessing cardiorespiratory fitness in clinical practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement From the American Heart Association. Circulation. 2016;134: e653–e699.
Nayor M, Xanthakis V, Tanguay M, Blodgett JB, Shah RV, Schoenike M, et al. Clinical and hemodynamic associations and prognostic implications of ventilatory efficiency in patients with preserved left ventricular systolic function. Circ Heart Fail. 2020;13: e006729.
Zheng G, Chen B, Fang Q, Lin Q, Tao J, Chen L. Baduanjin exercise intervention for community adults at risk of ischamic stroke: A randomized controlled trial. Sci Rep. 2019; 9:1240
Weishan X. The effect of health qigong baduanjin on cardiopulmonary function of aged people. J Bohai Univ Nat Sci Ed. 2013; 34:431–434.
Ma Z, Lei H, Tian K, Liu Z, Chen Y, Yang H, et al. Baduanjin exercise in the treatment of hypertension: A systematic review and meta-analysis. Front Cardiovasc Med. 2022; 9:936018.
Morisawa T, Kunieda Y, Koyama S, Suzuki M, Takahashi Y, Takakura T, et al. The relationship between sarcopenia and respiratory muscle weakness in community-dwelling older adults. Int J Environ Res Public Health. 2021; 18:13257.
Chmelo E, Nicklas B, Davis C, Miller GD, Legault C, Messier S. Physical activity and physical function in older adults with knee osteoarthritis. J Phys Act Health. 2013;10(6):777-783.
Phillips DB, Collins SÉ, Stickland MK. Measurement and interpretation of exercise ventilatory efficiency. Front Physiol. 2020; 11:659.
Lim YA, Boone T, Flarity JR, Thompson WR. Effects of qigong on cardiorespiratory changes: a preliminary study. Am J Chin Med. 1993;21(1):1-6.
Rascon J, Trujillo E, Morales-AcuÑa F, Gurovich AN. Differences between males and females in determining exercise intensity. Int J Exerc Sci. 2020; 13:1305-1316.
Ramos RA, Guimarães FS, Cordovil I, de Sa Ferreira A. The six-minute walk distance is a marker of hemodynamic-related functional capacity in hypertension: a case-control study. Hypertens Res. 2014; 37:746-752.
Lurati Buse GA, Mauermann E, Ionescu D, Szczeklik W, De Hert S, Filipovic M, et al. MET: Reevaluation for perioperative cardiac risk investigators; European Society of anaesthesiology and intensive care. Risk assessment for major adverse cardiovascular events after noncardiac surgery using self-reported functional capacity: international prospective cohort study. Br J Anaesth. 2023;130(6):655-665.
Wanderley FA, Oliveira J, Mota J, Carvalho MJ. Six-minute Walk distance (6MWD) is associated with body fat, systolic blood pressure, and rate-pressure product in community dwelling elderly subjects. Arch Gerontol Geriatr. 2011; 52:206-210.
Published:
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
