Sawitri Wanpen
School of Physical Therapy, Faculty of Associated Medical Sciences, Khon Kaen University, Khon Kaen, Thailand
Su Sandi Hla Tun
Human Movement Sciences, School of Physical Therapy, Faculty of Associated Medical Sciences, Khon Kaen University, Khon Kaen, Thailand
Nomjit Nualnetr
School of Physical Therapy, Faculty of Associated Medical Sciences, Khon Kaen University, Khon Kaen, Thailand
Uraiwan Chatchawan
School of Physical Therapy, Faculty of Associated Medical Sciences, Khon Kaen University, Khon Kaen, Thailand
Rungthip Puntumetakul
School of Physical Therapy, Faculty of Associated Medical Sciences, Khon Kaen University, Khon Kaen, Thailand
DOI: https://doi.org/10.14456/apst.2025.58
Keywords: Upper extremity chronic stoke impairment activity
Abstract
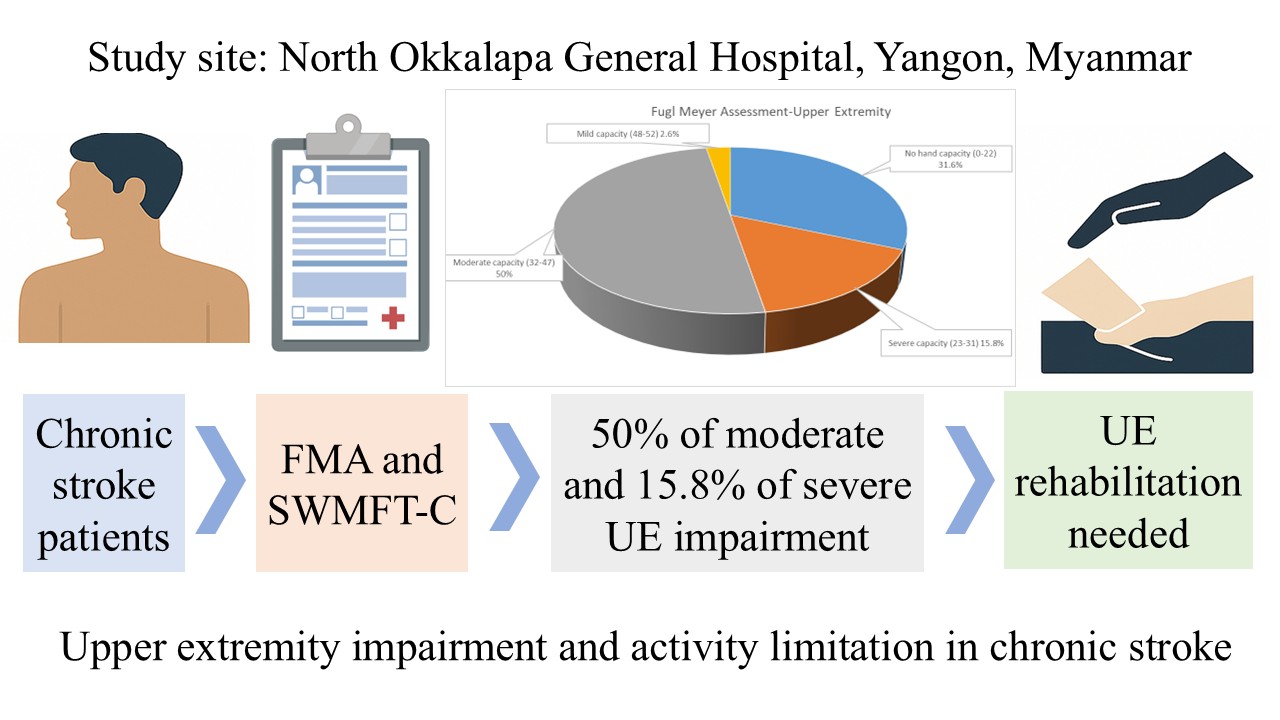
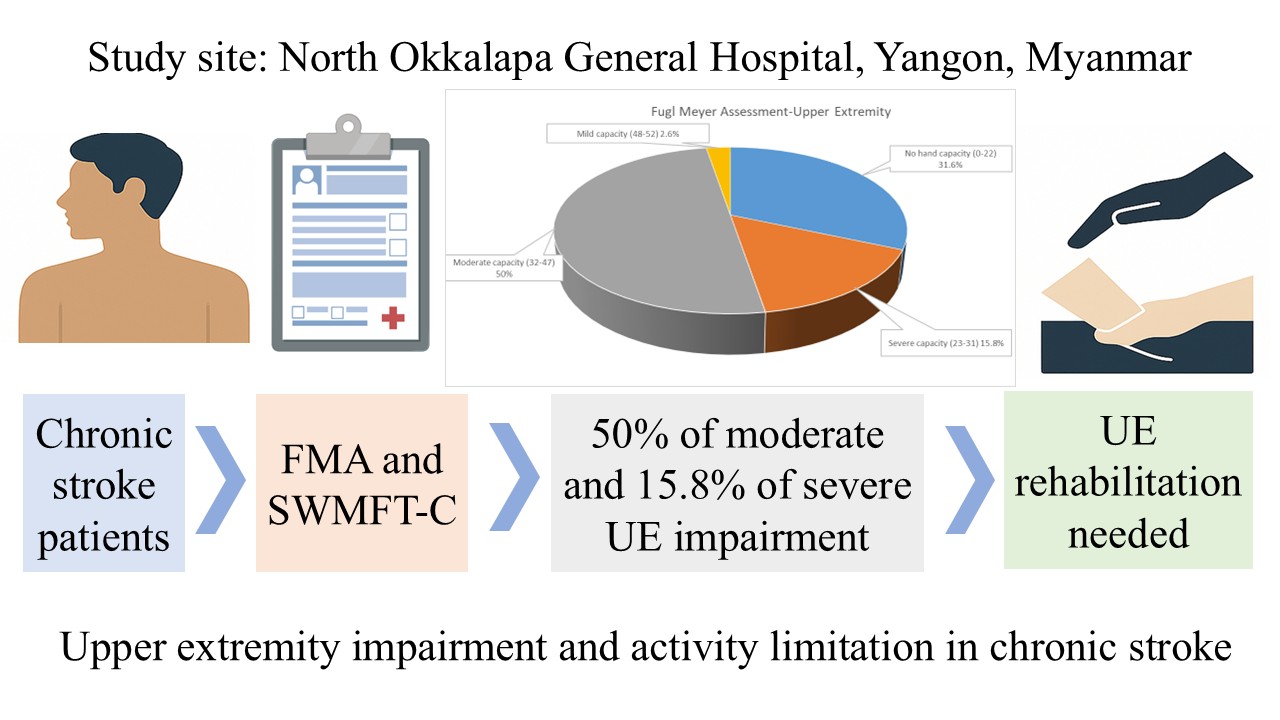
The objective of this study was to assess the proportion of upper extremity (UE) motor impairment and activity limitation in Myanmar individuals with chronic stroke and to find out the correlation between motor impairment and activity limitation. The research was conducted at North Okkalapa General Hospital, Yangon, Myanmar. The motor portion of Fugl-Meyer Assessment-Upper Extremity (FMA-UE) and Streamlined Wolf Motor Function Test for chronic stroke (SWMFT-C) were applied to assess the UE motor impairment and activity limitation. The result showed that 38 patients with chronic stroke were impaired in their UE functions (FMA-UE score of 7.0-52.0). Among these, four levels of impairments were demonstrated with full impairment (31.6%), severe impairment (15.8%), moderate impairment (50%), and mild impairment (2.6%). For the UE activities, the mean score (SD) of SWMFT-C performance time (s) was 7.52 seconds (6.00). The mean score (SD) of SWMFT-C functional ability scale (SWMFT-C-FAS) was 2.70 (1.12). In conclusion, the majority of the patients with chronic stroke were with moderate and severe motor impairment and activity limitation in their UE. Therefore, UE rehabilitation is needed to improve the impairments and functional recovery.
How to Cite
Wanpen, S., Hla Tun, S. S. ., Nualnetr, N., Chatchawan, U., & Puntumetakul, R. (2025). Determination of the proportion of severe impairment of the upper extremity functions in patients with chronic stroke. Asia-Pacific Journal of Science and Technology, 30(04), APST–30. https://doi.org/10.14456/apst.2025.58
References
Coscia M, Wessel MJ, Chaudary U, Millán J del R, Micera S, Guggisberg A, et al. Neurotechnology-aided interventions for upper limb motor rehabilitation in severe chronic stroke. Brain. 2019; 142(8): 2182-2197.
Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of stroke during 1990–2010: Findings from the Global Burden of Disease Study 2010. Lancet. 2014; 383(9913): 245-255.
Pei L, Zang XY, Wang Y, Chai QW, Wang JY, Sun CY, Zhang Q. Factors associated with activities of daily living among the disabled elders with stroke. Int J Nurs Sci. 2016; 3(1): 29-34.
Donkor ES. Stroke in the century: a snapshot of the burden, epidemiology, and quality of life. Stroke Res Treat. 2018; 2018: 1-10.
Allison R, Shenton L, Bamforth K, Kilbride C, Richards D. Incidence, time course and predictors of impairments relating to caring for the profoundly affected arm after stroke: a systematic review. Int J Physiother 2016; 21(4): 210-227.
Morris JH, Van Wijck F, Joice S, Donaghy M. Predicting health related quality of life 6 months after stroke: the role of anxiety and upper limb dysfunction. Disabil Rehabil. 2013; 35(4): 291-299.
Pollock A, St George B, Fenton M, Firkins L. Top ten research priorities relating to life after stroke. Lancet Neurol 2012; 11(3): 209.
Kristensen HK, Tistad M, Koch LV, Ytterberg C. The importance of patient involvement in stroke rehabilitation. PLoS One 2016: 11(6): 1-13.
Ward NS. Restoring brain function after stroke-bridging the gap between animals and humans. Nat Rev Neurol 2017; 13(4): 244-255.
Kwakkel G, Kollen BJ, Krebs HI. Effects of robot-assisted therapy on upper limb recovery after stroke: a systematic review. Neurorehabil Neural Repair. 2008; 22(2): 111-121.
Pekna M, Pekny M, Nilsson M. Modulation of neural plasticity as a basis for stroke rehabilitation. Stroke 2012; 43(10): 2819-2828.
Pike S, Lannin NA, Cameron L, Palit M, Cusick A. Chronic stroke survivors with upper limb spasticity: linking experience to the ICF. Disabil Rehabil 2021: 1-13.
Silva SM, Corrêa FI, de Morais Faria CD, Buchalla CM, da Costa Silva PF, Corrêa JC. Evaluation of post-stroke functionality based on the international classification of functioning, disability, and health: A proposal for use of assessment tools. J Phys Ther Sci 2015; 27(6): 1665-1670.
Poltawski L, Allison R, Briscoe S, Freeman J, Kilbride C, Neal D, et al. Assessing the impact of upper limb disability following stroke: a qualitative enquiry using internet-based personal accounts of stroke survivors. Disabil Rehabil 2016; 38(10): 945-951.
Junmee C, Siriwachirachai S, Chompoonimit A, Chanavirut R, Thaweewannakij T, Nualnetr N. Health status of patients with stroke in Ubolratana District, Khon Kaen Province: International Classification of functioning, disability and health-based assessments. Thai J Phys Ther 2021; 43(1): 45-63. [in Thai].
Seephim B, Srisoparb W, Nualnetr N. Upper limb functions and complications of hemiplegic side in patients with chronic stroke in the community. Srinagarind Med J 2020; 35(1): 51-58. [in Thai].
Srisoparb W, Nualnetr N, Sommanochai K, Karinta N, Charungthanakij P. Functional abilities of the upper limbs in people with chronic cerebrovascular disease in the community of Naresuan University Hospital. Thai J Phys Ther 2020; 41(2): 60-74. [in Thai].
Hijikata N, Kawakami M, Ishii R, Tsuzuki K, Nakamura T, Okuyama K, et al. Item difficulty of fugl-meyer assessment for upper extremity in persons with chronic stroke with moderate-to-severe upper limb impairment. Front Neurol 2020; 11(1395): 1-9.
Potter TB, Tannous J, Vahidy FS. A contemporary review of epidemiology, risk factors, etiology, and outcomes of premature stroke. Curr. Atheroscler. Rep 2022; 24(12): 939-948.
Winkelmeier L, Kniep H, Faizy T, Heitkamp C, Holtz L, Meyer L, et al. Age and functional outcomes in patients with large ischemic stroke receiving endovascular thrombectomy. JAMA Netw Open 2024; 7(8): 1-11.
Daniel WW, Cross CL. Biostatistics: A foundation for Analysis in the health Science. 10th ed. Hoboken: Rosatone; 2013.
Gladstone DJ, Danells CJ, Black SE. The Fugl-Meyer assessment of motor recovery after stroke: a critical review of its measurement properties. Neurorehabil Neural Repair 2002; 16(3): 232-240.
Hoonhorst MH, Nijland RH, Van Den Berg JS, Emmelot CH, Kollen BJ, Kwakkel G. How do Fugl-Meyer arm motor scores relate to dexterity according to the action research arm test at 6 months poststroke? Arch Phys Med Rehabil 2015; 96(10): 1845-1849.
Chen HF, Wu CY, Lin KC, Chen HC, Chen CP, Chen CK. Rasch validation of the streamlined wolf motor function test in people with chronic stroke and subacute stroke. Phys Ther 2012; 92(8): 1017-1026.
Hodics TM, Nakatsuka K, Upreti B, Alex A, Smith PS, Pezzullo JC. Wolf Motor Function Test for characterizing moderate to severe hemiparesis in stroke patients. Arch Phys Med Rehabil 2012; 93(11): 1963-1967.
Banjai RM, Freitas SM, Silva FP, Alouche SR. Individuals’ perception about upper limb influence on participation after stroke: An observational study. Top Stroke Rehabil 2018; 25(3): 174-179.
Faria-Fortini I, Michaelsen SM, Cassiano JG, Teixeira-Salmela LF. Upper extremity function in stroke subjects: relationships between the international classification of functioning, disability, and health domains. J Hand Ther 2011; 24(3): 257-265.
Hensel L, Lange F, Tscherpel C, Viswanathan S, Freytag J, Volz LJ, Eickhoff SB, Fink GR, Grefkes C. Recovered grasping performance after stroke depends on interhemispheric frontoparietal connectivity. Brain 2023; 146(3): 1006-1020.
Published:
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
